A slow progression of kidney damage or kidney disease is referred to as chronic kidney disease (CKD). This disease usually does not show any significant symptoms at the beginning but as it progresses early signs start appearing. As per the National Kidney Foundation, CKD mostly remains asymptomatic until reaching kidney failure. The disease cannot be treated permanently, it can be controlled to prevent its growth and reduce its complications.
Chronic kidney disease is also known as chronic renal disease, chronic kidney failure, or chronic renal failure. As per the statistics, CKD affects 37 million Americans and is a significant public health problem in the U.S.
In medical terms, CKD is defined as a progressive deterioration in kidney function continued for more than 3 months, which is further classified into different stages of chronic kidney disease depending upon the degree of kidney damage. The stages of CKD can be identified by measuring the Glomerular Filtration Rate (GFR) and the level of proteinuria.
Chronic Kidney Disease Stages and Symptoms:
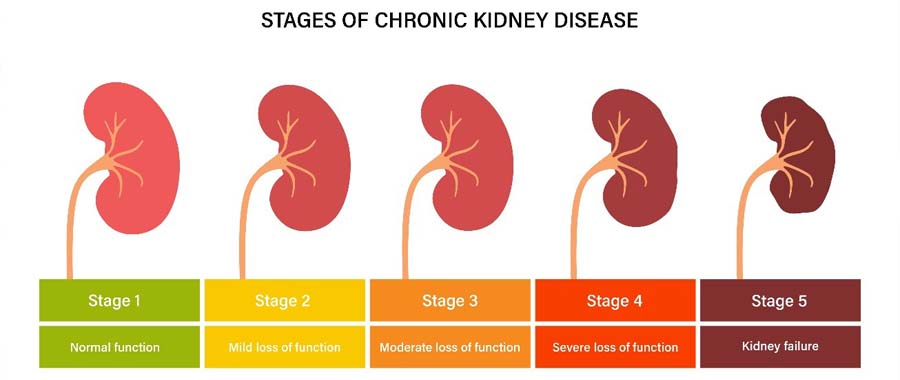
A chronic kidney disorder is classified into 5 stages where the final stage is End-Stage Renal Disease (ESRD). A doctor assesses the patient’s eGFR (Estimated Glomerular filtration rate), which shows how well kidneys are functioning to remove waste products from the blood and determine the stage of kidney disease.
CKD Stage 1: GFR (ml/min) value 90 and above
This is the beginning of kidney disease, where kidneys are healthy and working well, but there might be some mild symptoms that can be detected at this stage.
Symptoms: Protein, creatinine, or urea in urine, swelling in legs, urinary tract infection, high blood pressure, etc., can be detected at this stage.
CKD stage 2: GFR (ml/min) between 60 to 89
This is the second stage of chronic kidney disease. At this stage, the eGFR value is considered normal and kidneys are also functioning well, but there are some visible symptoms that can be observed.
Symptoms: Fatigue, itchy skin, loss of appetite or sleep, weakness, pain in the lower back, increased or decreased urination, etc.
CKD Stage 3A and 3B: GFR (ml/min) between 45 to 59 and 30 to 44 respectively
When eGFR drops between 30 to 59, kidney disease is considered to reach stage 3 where there is a significant reduction in the filtration of waste products by kidneys from blood. Stage 3 chronic kidney disease further classified into two that is stage 2A, when eGFR lies between 45 to 59, and stage 3B when eGFR lies between 30 to 44.
Symptoms: Shortness of breath, kidney pain felt in back, fluid retention, change in urine color (foamy, dark orange, brown, tea color or red), muscle cramp at night, insomnia, fatigue, and weakness, etc.
Frequently asked questions at stage 3 of chronic kidney disease:
Q: Is CKD stage 3 reversible?
A: There is no cure for damaged kidneys at any stage, but we can control its further progression as efficiently as it is detected at earlier stages. Likewise, at stage 3 a doctor always tries to prevent further complications and growth of kidney disease from stage 3 to stage 4 and 5.
Q: What is the life expectancy of someone with stage 3 kidney disease?
A: On average, the life expectancy of a male patient, who is 40, at CKD stage 3, is 24 years, whereas for a female patient of the same age group, is 28 years. In a 10-year study, it has been found that half of the patients at stage 3 progressed to further stages of the disease. If CKD is diagnosed and managed at an early stage, then a patient at stage 3 can have a longer life expectancy than stages 4 and 5.
Q: Does Stage 3 kidney disease always progress?
A: As per the studies and statistics half of the CKD stage 3 patients progressed to the next stages of the disease.
Q: What foods should I avoid with CKD Stage 3?
A: A person with CKD stage 3, must avoid certain foods in their diet to control the further progression of the disease. These foods include:
- Processed meat.
- Dark-colored sodas.
- High potassium diets like bananas, avocados, apricots, kiwifruit, and oranges, etc.
- Food that increases blood sugar like dry fruits, potatoes, sweet potatoes, food added with artificial sweetener, snack food, fruit juice, etc.
- Certain green leafy vegetables like spinach, beet greens, chard, etc.
- Packaged foods, instant meals, and fast food.
- Most beans and lentils.
CKD Stage 4: GFR (ml/min) between 15 to 29
At stage 4 of chronic kidney disease, the patient’s kidney filtration capacity is reduced by a significant amount, causing accumulation of waste products in the blood leading to a disease called uremia. At this stage patient likely to develop other chronic diseases as well like cardiovascular disease, anemia, high blood pressure, bone disease, etc., and need to consult a nephrologist on every 3 months for routine checkup and monitoring. Here a nephrologist explains and educates further treatment options of dialysis or transplant to the patient to make a decision.
Symptoms: Kidney pain felt in the back, nerve problem (tingling sensation at toes and fingers), shortness of breath, fluid retention at extremities, nausea/ vomiting, bad breath, difficulty concentrating, insomnia, restless legs, loss of appetite, etc.
CKD Stage 5 or Kidney Failure: GFR (ml/min) less than 15
CKD stage 5 is diagnosed, when a patient’s kidney reached very close to failure or stopped filtration completely (completely failed). This stage is called End-Stage Kidney Disease (ESRD). At this stage, patients’ blood accumulates lots of impurities which further damage the kidneys and cause additional complications that hinder regulation of blood pressure, inhibit hormone erythropoietin from making blood cells, reduced activation of vitamin D to maintain healthy bones, etc.
Symptoms: not enough urination, pain or stiffness or swelling of joints, unintended weight loss, a loss of sense of taste, difficulty sleeping, weakness or numbness, headache, nose bleeding, fluid retention in feet and ankle, itchiness, bruising easily, etc.
CKD Treatment and Management:
Chronic kidney disease treatment and management is a long ongoing process. It has been found that there is no permanent cure for CKD, but if detected at an early stage and depending on underlying causes, CKD can be controlled or treated. A nephrologist primarily focuses on controlling underlying causes, the lifestyle of the patient, medication to treat complications, dialysis, and kidney transplant while managing or treating a chronic kidney disease patient.

Controlling Underlying causes and complications
Diseases like high blood pressure, diabetes, high cholesterol, autoimmune disease, etc. are major reasons for developing CKD in a person. Treatment of these diseases can be an effective procedure to control the progression of CKD and related complications. Besides this medication for relieving swelling, anemia, protection of bones, and lowering intake of protein in the diet are included in CKD treatment.
Focus on lifestyle changes of the patient.
A CKD patient is required to make some lifestyle changes during and after treatment, which are below:
- Quit tobacco or cigarettes.
- Restrict salt intake, less than 6gms in a day.
- Exercise for at least 30 mins.
- Maintain a healthy weight.
- Adopt a healthy eating habit.
- Avoid having nephrotoxins, non-steroidal anti-inflammatory drugs (NSAIDs), etc.
Treatment of End-Stage Kidney Disease (ESRD):
Once a patient’s kidney reaches CKD stage 5 or end-stage kidney disease, it stops completely filtering waste from the blood. At this stage, the patient needs dialysis or a kidney transplant as a treatment plan. A doctor will explain various available dialysis options and kidney transplant procedures so that a patient can understand and make his mind or choose a particular treatment option.

Types of Dialysis:
Dialysis is a process in which the extra fluid or waste toxic products are removed from the blood keeping a balance of certain chemicals such as potassium, phosphorus, sodium, and bicarbonate, etc. and controlling high blood pressure artificially using a machine.
There are two types of dialysis: Hemodialysis and peritoneal dialysis.
Hemodialysis:
In this process, an artificial kidney called a hemodialyzer is used to removed waste toxic products from the blood. The doctor makes access into your blood vessel by doing minor surgery to your arm or leg or may require developing a fistula (joining artery and vein). The hemodialysis process lasts for 4 hours and needs to be done 3 times a week. For a faster process, a method called high-flux dialysis is also available, which can be done as prescribed by your doctor.
There are 2 types of hemodialysis: In-center hemodialysis and home hemodialysis.
Peritoneal Dialysis:
In this process, the blood is cleaned within the body using a catheter (a plastic tube) placed into the patient’s abdomen to make an access. The catheter slowly filled with dialysate and clean blood that flows through arteries and veins in the abdomen passing into the dialysate.
There are two types of peritoneal dialysis: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD).
Kidney Transplant:
A kidney transplant is the best treatment option for people with end-stage kidney disease and is very safe and successful. In this process, a person may undergo a kidney transplant surgery and a healthy kidney is implanted in him. A successful kidney transplant depends on how you take care of yourself after your transplant and following your doctor’s orders after the transplant.