The human body is a marvel of interconnected systems, each playing a vital role in maintaining our overall health. Among these, the kidneys are unsung heroes, quietly working to filter waste and excess fluids from our blood, regulate blood pressure, and keep electrolytes in balance. But what happens when the very vessels responsible for supplying blood to these essential organs become compromised? This is where renovascular disease enters the scene. In this comprehensive overview, we will explore the intricacies of renovascular disease, delving into its causes, symptoms, diagnosis, treatment options, and the crucial role of lifestyle modifications in managing this condition.
Unveiling Renovascular Disease
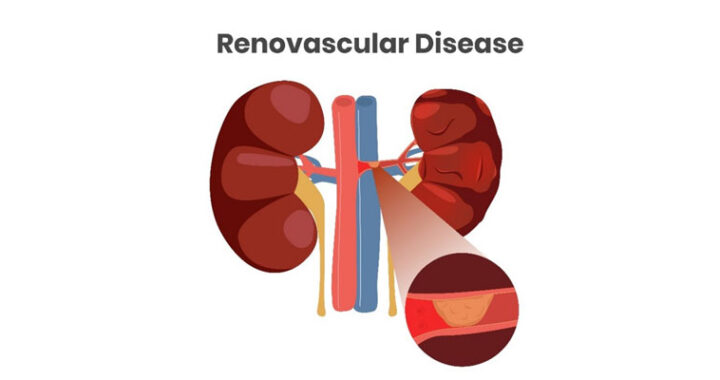
Renovascular disease, also known as renal artery disease, is a vascular condition that primarily affects the renal arteries, the blood vessels responsible for delivering blood to the kidneys. It is a condition that can remain silent for years, quietly progressing until it reaches an advanced stage, potentially causing severe health issues. To understand renovascular disease better, let’s explore its causes and risk factors.
Causes of Renovascular Disease
- Atherosclerosis: The most common cause of renovascular disease is atherosclerosis, a condition characterized by the buildup of plaque inside the arteries. This plaque consists of cholesterol, fatty deposits, and other substances that accumulate over time, gradually narrowing the renal arteries. As these arteries become constricted, blood flow to the kidneys diminishes.
- Fibromuscular Dysplasia (FMD): While less common, fibromuscular dysplasia is another cause of renovascular disease. This condition involves abnormal cell growth in the arterial walls, leading to the narrowing of the renal arteries and compromised blood flow.
Risk Factors for Renovascular Disease
Several factors increase the risk of developing renovascular disease, including:
- Smoking: Smoking is a major contributor to atherosclerosis, which is the primary cause of renal artery disease.
- High Blood Pressure: Hypertension (high blood pressure) is both a risk factor and a consequence of renovascular disease. The condition can cause damage to the renal arteries, exacerbating the problem.
- Diabetes: Individuals with diabetes are at an increased risk of atherosclerosis, which can indirectly lead to renovascular disease.
- Family History: A family history of kidney disease or renovascular disease may raise your susceptibility to this condition.
Symptoms of Renovascular Disease
One of the challenges in diagnosing renovascular disease is its often-silent progression. Many individuals do not experience symptoms until the disease has reached an advanced stage. Symptoms, if they arise, could comprise:
Hypertension (High Blood Pressure): Uncontrolled high blood pressure, often resistant to medication, can be a hallmark symptom of renovascular disease.
- Fluctuations in Blood Pressure: Blood pressure may vary significantly between arms, with one arm showing higher readings than the other.
- Decreased Kidney Function: As the condition worsens, it can lead to a decrease in kidney function. This may result in symptoms such as fatigue, swelling in the legs and ankles (edema), and changes in urination patterns.
- Abdominal or Flank Pain: In some cases, individuals with renovascular disease may experience abdominal or flank pain, often due to reduced blood flow to the kidneys.
It’s important to note that many of these symptoms are nonspecific and can be attributed to other medical conditions. If you experience any of these symptoms, especially if you have risk factors for renovascular disease, it’s essential to consult a healthcare professional for a proper evaluation.
Diagnosing Renovascular Disease
Diagnosing renovascular disease is a multifaceted process that involves a combination of medical history assessment, physical examination, and specialized diagnostic tests. These tests help confirm the presence of the disease, determine its severity, and guide treatment decisions. Common diagnostic methods include:
- Renal Ultrasound: A non-invasive imaging technique that uses sound waves to create images of the kidneys and renal arteries.
- Magnetic Resonance Angiography (MRA): An imaging test that provides detailed images of the renal arteries using magnetic resonance technology.
- Computed Tomography Angiography (CTA): A specialized X-ray test that produces detailed cross-sectional images of the renal arteries.
- Renal Artery Angiography: A more invasive procedure where a contrast dye is injected into the renal arteries, allowing for clear X-ray visualization.
Treatment Options for Renovascular Disease
The choice of treatment for renovascular disease depends on the severity of the condition and the individual’s overall health. Treatment options include:
- Lifestyle Modifications: For individuals with mild renovascular disease or those at risk, lifestyle changes can be highly effective. These changes may include a heart-healthy diet low in sodium and saturated fats, regular exercise, smoking cessation, and stress management.
- Medications: Blood pressure medications, such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs), may be prescribed to help manage hypertension and protect the kidneys.
- Angioplasty: In cases where the renal arteries are significantly narrowed, a minimally invasive procedure called angioplasty may be performed. During angioplasty, a small balloon is inflated in the narrowed artery to widen it and improve blood flow.
- Stent Placement: In conjunction with angioplasty, a stent—a small mesh tube—may be inserted to keep the renal artery open and prevent it from collapsing.
- Surgery: In severe cases where other interventions are not effective, surgical revascularization may be considered. This involves bypassing the blocked portion of the renal artery with a graft or rerouting blood flow through a new pathway.
The choice of treatment is highly individualized and should be discussed with a healthcare provider, considering factors like the patient’s age, overall health, and the severity of the disease.
Lifestyle Changes and Renovascular Disease Management
Regardless of the chosen treatment approach, lifestyle modifications play a crucial role in managing renovascular disease. Consider these important lifestyle changes:

Dietary Modifications: Adopting a heart-healthy diet can help manage blood pressure and improve kidney function. Focus on consuming foods low in sodium, saturated fats, and processed sugars. Elevate your consumption of fruits, vegetables, whole grains, and lean proteins.

Regular Exercise: Engage in regular physical activity to help control weight and maintain cardiovascular health. Consult with your healthcare provider before starting any exercise program, especially if you have other medical conditions.
- Smoking Cessation: If you smoke, quitting is one of the most impactful changes you can make to improve your overall health. Smoking cessation is crucial, as smoking is a major risk factor for renovascular disease and exacerbates its effects.
- Stress Control: Prolonged stress may be a factor in elevated blood pressure. Integrate stress-relief practices into your daily regimen, such as meditation, deep breathing exercises, or yoga.
- Medication Adherence: If your healthcare provider prescribes medication, take it as directed and attend regular follow-up appointments to monitor your progress.
Renovascular disease is a multifaceted condition that demands attention, early diagnosis, and proactive management. Understanding its causes, symptoms, diagnosis, and treatment options is crucial for individuals at risk and those living with the condition. Furthermore, embracing a heart-healthy lifestyle and seeking support from healthcare professionals from Clinical Renal Associates can significantly enhance the quality of life for individuals with renovascular disease. As medical research continues to advance, there is hope for better outcomes and a brighter future for those affected by this condition.