
What is Chronic Kidney Disease (CKD)?
Finding out you have chronic kidney disease (CKD) might feel overwhelming at first but knowing more about it can help you feel more in control of your diagnosis. CKD happens when your kidneys slowly lose their ability to function as well, they should. This means they can’t filter waste and extra fluids from your blood. Since early CKD often has no symptoms, frequent check-ups are crucial for early detection and effective management of CKD.
What Causes CKD?
Several things can lead to CKD, including:
- Diabetes: High blood sugar can damage the tiny filters in your kidneys.
- High Blood Pressure: This can hurt your kidneys’ blood vessels.
- Glomerulonephritis: This is a condition where the tiny filters (called glomeruli) in your kidneys become inflamed.
- Polycystic Kidney Disease: A genetic condition that causes cysts to form in your kidneys.
- Urinary Tract Obstructions: Blockages like kidney stones can cause lasting damage if they happen often.
- Recurrent Kidney Infections: Frequent infections can leave scars on your kidneys.

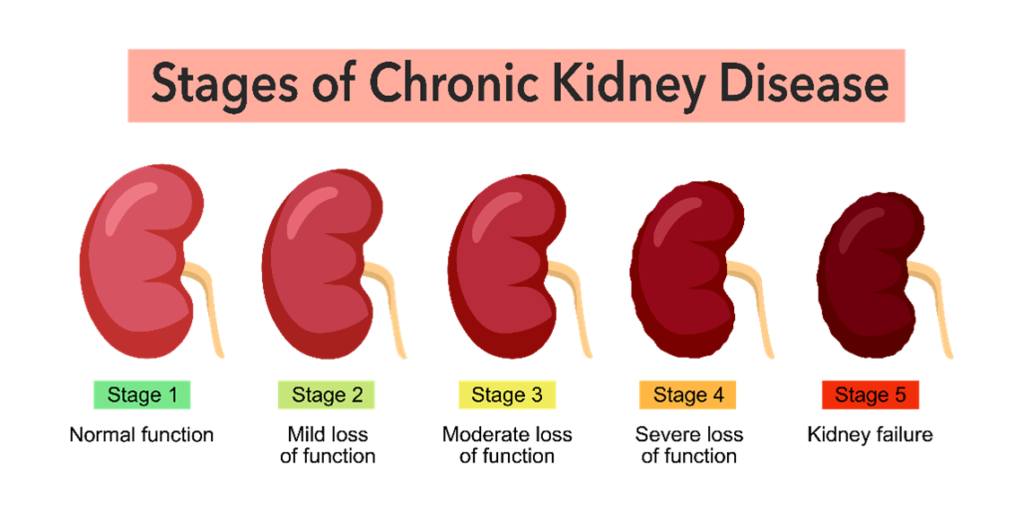
What are the Stages of CKD?
CKD progresses through five stages, measured by a blood test called glomerular filtration rate, or GFR. Familiarizing yourself with the stages can give you a clearer idea of what to anticipate:
- Chronic Kidney Disease Stage 1: Minimal kidney damage with normal function (GFR 90+). Often no symptoms.
- Chronic Kidney Disease Stage 2: Mild kidney impairment with a small decrease in function (GFR 60-89). Symptoms are rare or mild.
- Chronic Kidney Disease Stage 3: Moderate damage (GFR 30-59). You might feel tired or notice changes in your urine. This stage is split into 3A (GFR 45-59) and 3B (GFR 30-44).
- Chronic Kidney Disease Stage 4: Severe damage (GFR 15-29). Symptoms become more noticeable, like anemia or bone disease.
- Chronic Kidney Disease Stage 5: Kidney failure (GFR less than 15). Dialysis or a kidney transplant becomes required.
How is CKD Diagnosed?
To find out if you have CKD, your doctor might use:
- Blood Tests: These measure your creatinine levels to estimate your GFR.
- Urine Tests: Check for protein or blood in your urine.
- Imaging Tests: Ultrasounds or CT scans give a picture of your kidneys.
- Kidney Biopsy: Sometimes, a small tissue sample is needed to see how much damage there is and why it’s happening.
How to Manage CKD
Living with CKD means making some changes and keeping a close eye on your health:
- Regular Monitoring: Keep up with your doctor’s appointments to check your kidney function.
- Medications: Take any prescribed medicines to control blood pressure, blood sugar, and other medical conditions.
- Lifestyle Changes: Eating a kidney-friendly diet, exercising, and avoiding smoking and excessive alcohol can make a big difference.
- Specialized Care: Working with a kidney specialist (nephrologist) can help you get the best care.

Foods for CKD
Your diet plays a significant role in maintaining kidney health:
- Good Foods:
- Fresh Fruits and Vegetables: These are low in sodium and good for your overall health. Your doctor might advise you to avoid high-potassium fruits like bananas, if your potassium is too high.
- Lean Proteins: Chicken, fish, and tofu are easier on your kidneys.
- Whole Grains: Brown rice, oatmeal, and whole wheat bread are nutritious without overloading your kidneys.
- Foods to Avoid:
- Processed Foods: These are high in sodium, which can be hard on your kidneys.
- High-Sodium Foods: Chips, pretzels, and canned soups should be limited.
- Phosphorus-Rich Foods: Dairy products, nuts, and certain soft drinks can strain your kidneys.
Treating CKD
The treatment approach varies based on the stage of your CKD:
- Early Stages:
- Lifestyle Changes: Healthy eating and regular exercise can slow down CKD.
- Medications: Managing conditions like high blood pressure and diabetes are crucial. Your nephrologist will often give you medications that help protect your kidneys.
- Advanced Stages:
- Kidney Transplant: A new kidney from a donor can be a more permanent solution.
- Dialysis: This treatment helps remove waste and extra fluids from your blood.
Potential Complications if CKD Worsens
If CKD progresses, it can lead to other health issues:
- High Blood Pressure: CKD can lead to hypertension, which can further harm your kidneys.
- Anemia: Reduced kidney function can lead to lower red blood cell production.
- Weak Bones: CKD can affect the balance of calcium and phosphorus, resulting in bone disease.
- Nerve Damage: Waste build-up can damage your nerves, causing tingling or numbness.
- Cardiovascular Disease: CKD increases your risk for heart disease and stroke.
- Kidney Failure: In later stages, CKD can progress to kidney failure, requiring dialysis or a kidney transplant.
Preventing CKD
You can help prevent CKD by:
- Managing Risk Factors:
- Blood Pressure: Keep it under control with lifestyle changes and medications if needed.
- Blood Sugar Levels: Properly control diabetes to protect your kidneys from damage.
- Healthy Lifestyle:
- Regular Exercise: Supports overall health and weight management.
- Balanced Diet: Eat low-sodium foods rich in fruits, vegetables, and whole grains.
- Stay Hydrated: Adequate water intake supports proper kidney function.
- Avoid Tobacco Products: Quitting smoking can significantly reduce your risk of CKD.
- Regular Screenings: Annual health check-ups can help detect early signs of kidney problems and allow for timely intervention.

Finding out you have CKD might seem scary, but with the right care and lifestyle changes, you can manage it effectively. Stay positive, follow your doctor’s advice, and take steps to maintain a healthy lifestyle. You don’t have to face this alone – the team at Clinical Renal Associates is here to support you at every step. Request an appointment with our top-rated providers today,
