In the intricate web of bodily functions, maintaining fluid balance is crucial for overall health and well-being. However, disruptions in this balance can lead to conditions like hypervolemia, also known as fluid overload. This blog seeks to illuminate the subject, addressing its symptoms, origins, diagnosis, and approaches to management.
What is Hypervolemia?
It is a medical condition characterized by an excessive accumulation of fluid in the extracellular space of the body. This fluid overload can occur in various compartments, including the intravascular (blood vessels) and interstitial (tissues surrounding cells) spaces. While the human body is adept at regulating fluid balance through mechanisms such as osmoregulation and the renin-angiotensin-aldosterone system, certain factors can disrupt this delicate equilibrium, leading to hypervolemia.
 Symptoms:
Symptoms:
Identifying hypervolemia can be challenging, as symptoms may vary depending on the severity of fluid overload and underlying health conditions. However, common signs and symptoms include:
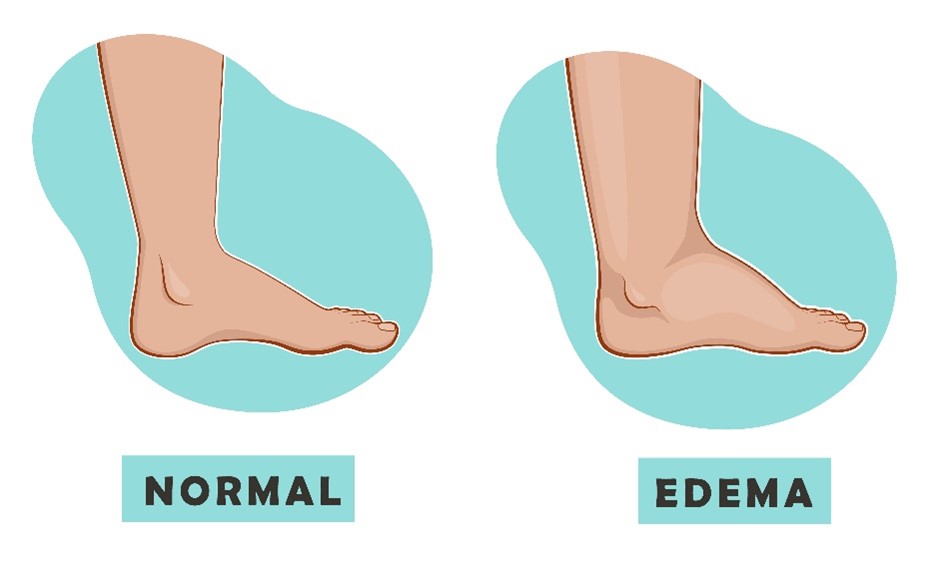
- Swelling (Edema): Excessive fluid accumulation can cause swelling in various parts of the body, such as the legs, ankles, or abdomen. This swelling may be particularly noticeable at the end of the day or after prolonged periods of sitting or standing.
- Shortness of Breath (Dyspnea): Fluid overload can exert pressure on the lungs, making it difficult to breathe. Individuals may experience breathlessness, especially when lying flat or during physical exertion.
- Weight Gain: Rapid and unexplained weight gain is a hallmark symptom. This weight gain is primarily due to the retention of fluid rather than an increase in body fat.
- Fatigue: Excessive fluid accumulation can impair circulation and oxygen delivery to tissues, leading to feelings of fatigue and lethargy.
- Increased Blood Pressure: It can elevate blood pressure levels, putting additional strain on the heart and blood vessels.
- Decreased Urine Output: In severe cases, it may lead to a decrease in urine production, indicating impaired kidney function.
Causes:
Hypervolemia can arise from various underlying conditions and factors that disrupt the body’s fluid balance. Some common causes include:
- Heart Failure: In congestive heart failure, the heart’s ability to pump blood efficiently is compromised, leading to fluid accumulation in the lungs and peripheral tissues.
- Kidney Dysfunction: Conditions such as chronic kidney disease or acute kidney injury can impair the kidneys’ ability to regulate fluid and electrolyte balance, resulting in fluid retention.
- Liver Cirrhosis: Liver cirrhosis can lead to portal hypertension and hypoalbuminemia, contributing to fluid accumulation in the abdomen (ascites) and other parts of the body.
- Excessive Sodium Intake: High dietary sodium intake can increase fluid retention in the body.
- Certain Medications: Some medications, such as corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), can cause fluid retention as a side effect.
- Endocrine Disorders: Hormonal imbalances, such as those seen in Cushing’s syndrome or hyperaldosteronism, can disrupt fluid balance and contribute to fluid overload.
- Intravenous Fluid Administration: Excessive administration of intravenous fluids, particularly in hospitalized patients, can lead to fluid overload if not properly monitored.

Diagnosis and Tests:
Diagnosing hypervolemia typically involves a comprehensive assessment by healthcare professionals, including a thorough medical history, physical examination, and diagnostic tests. Key diagnostic steps may include:
- Medical History: The healthcare provider will inquire about symptoms, medical history, current medications, and any underlying health conditions that may contribute to fluid retention.
- Physical Examination: A physical examination may reveal signs of fluid overload, such as swelling (edema), increased jugular venous pressure, or abnormal lung sounds.
- Laboratory Tests: Blood tests may be performed to assess kidney function (serum creatinine, blood urea nitrogen), electrolyte levels (sodium, potassium), and markers of heart function (BNP or NT-proBNP).
- Imaging Studies: Imaging tests, such as chest X-rays or echocardiography, may be conducted to evaluate the heart, lungs, and fluid distribution within the body.
- Urinalysis: Urinalysis may help assess kidney function and detect abnormalities such as proteinuria or hematuria.
- Electrocardiogram (ECG): An ECG may be performed to evaluate heart rhythm and identify any cardiac abnormalities.
Management and Treatment:
Effective management of hypervolemia involves addressing underlying causes, relieving symptoms, and preventing complications. Treatment strategies may include:
- Treating Underlying Conditions: Targeted treatment of underlying conditions such as heart failure, kidney disease, or liver cirrhosis is essential to manage fluid overload effectively.
- Diuretics: Diuretic medications, such as loop diuretics (e.g., furosemide) or thiazide diuretics, may be prescribed to increase urine output and reduce fluid retention.
- Dietary Modifications: Restricting dietary sodium intake can help reduce fluid retention in individuals with hypervolemia. Healthcare providers may also recommend limiting fluid intake, particularly in cases of severe fluid overload.
- Fluid and Electrolyte Management: Monitoring fluid and electrolyte levels is crucial, especially in patients receiving diuretic therapy or intravenous fluids.
- Lifestyle Modifications: Encouraging lifestyle modifications such as regular exercise, weight management, and smoking cessation can help improve overall cardiovascular health and reduce the risk of fluid overload.
- Medication Adjustment: Adjusting the dosage or discontinuing medications that contribute to fluid retention (e.g., corticosteroids, NSAIDs) may be necessary under medical supervision.
- Monitoring and Follow-Up: Regular monitoring of symptoms, fluid status, and response to treatment is essential to optimize management and prevent recurrence.
Hypervolemia is a complex medical condition characterized by fluid overload, with diverse underlying causes and manifestations. Early recognition, accurate diagnosis, and appropriate management are paramount in mitigating the associated risks and improving patient outcomes. Collaboration between patients, healthcare providers, and multidisciplinary teams is essential to tailor treatment strategies to individual needs and promote optimal fluid balance and overall well-being.